Help more babies receive life-saving donor milk
Amelia was born 3 months prematurely and received donor milk in neonatal intensive care. Watch the video to hear her parents Kay and Ross tell her amazing story.
DONATE NOWWe rely upon the generosity and goodwill of our supporters to be able to continue providing this life-changing service to families. Every pound donated really does make a difference, please help if you can.
Pays for one milk donor onboarding pack
Feeds a premature baby with donor milk for a day
Helps our volunteers deliver donor milk for a week
Recruits one new milk donor, whose milk would feed on average 20 babies
Amelia was born 3 months prematurely and received donor milk in neonatal intensive care. Watch the video to hear her parents Kay and Ross tell her amazing story.
DONATE NOWEvery day our growing team is racing to help more hospitals, more families and more projects that spread knowledge about human milk. Get in touch if you can help!
Hospitals we work with
Babies supported with donor milk
Milk donors recruited
Litres of donor milk provided
Koan was born with a rare genetic condition and received donor milk from the HMF. Watch Koan’s parents - Shurron and Kel tell their amazing story.
WATCH VIDEO OF KOAN'S STORY
We are excited to announce the launch of Connecting Hearts – a collaboration between the HMF, Swansea University and artist Leanne Pearce. Through a series of beautiful paintings & audio, the incredible stories behind those involved in receiving, donating and supporting human milk banking are told, bringing to life the profound impact that milk donation can have for families, as a beacon of hope for those affected by infant prematurity, baby loss, maternal cancer and more. Each painting sheds light on a new perspective, connecting us with the kindness and shared humanity that underpins milk banking services. The event will be hosted at the Taliesin Arts Centre – it will start at 6.30pm with an opportunity to view the paintings and have a drink from the bar. The main event in the auditorium is from 7.30pm – 9pm with further opportunity to view the paintings and talk to speakers afterwards. We are grateful to HEFCW Research Wales Innovation Funding and UKRI for supporting this event and painting series.

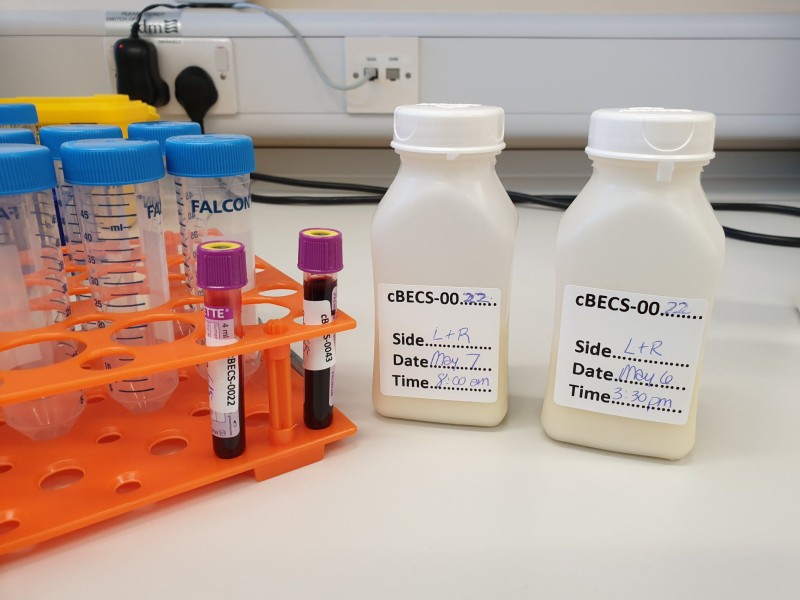
In our first five years the Human Milk Foundation has pasteurised over 17,000 litres of donor milk, supplying over 50 NHS hospital neonatal units and helping save thousands of tiny lives. Behind every drop of donor milk is a story, and many acts of kindness. From the amazing individuals who take the time and care to express and donate their milk, the dedicated Blood Bikers who are out on the roads every day ensuring the milk gets to the babies who need it, our wonderful volunteers who help support these collections and run our network of hubs, our charity partners and collaborators, to every single person who has contributed and raised vital funds to support our growth. We simply couldn’t run this life-saving service without you all – and together we are making a difference to families one by one.
So, we wanted your words to tell the story of our 5 years. We’ve been overwhelmed with the incredible response, the lovely messages, videos, and photos that you’ve shared with us and we really are so very grateful to each and every one of you for your support, without which we would not have reached this milestone. Take a look at our 5 year impact video and celebration messages on our special page.

We were so excited to launch our brand new HMF gift store on World Day of Human Milk Donation – www.hmfgifts.com
Our online shop includes beautiful mugs, canvas tote bags, eco-phone covers and other practical items featuring designs based on human milk science, supporting parents, and the snowdrop flower – our charity emblem. All of our products are made exclusively in the UK and printed on demand using sustainable Epson dye-sublimation printing technology. Proceeds from products purchased in the store help us to support more babies with donor milk.
Watch this space for more products and designs coming soon!
Human milk is a remarkable fluid, changing by the minute, hour, day and season to respond to the needs of the developing baby. Milk adapts to protect babies from infections in their environment, supplies stem cells and immune cells from the mother, and patterns the development of every organ in the body. Yet human milk is full of unknowns.
Our commitment to scientific discovery not only aims to help families understand the magic of milk, but make sure that milk banking processes are continually innovating and improving.